“Dear HER-Health” with Heather Florio
Dear HER-Health,
I’m 52 and noticed I’ve entered perimenopause — more frequent night sweats, mood swings, and lately a new symptom: my pelvic floor feels weaker, I’m getting urgent urination at odd times, and sex has become uncomfortable with less lubrication and more “drag.” I also haven’t had a period in about a year, though I know technically I’m probably in menopause. I’m nervous about starting hormone-therapy (HRT) because I read a few scary headlines about risks, and yet I feel like something has to change. Where do I even begin — for the hot flashes, bladder/urgency issues, and sexual changes? What questions should I ask my doctor? Are there non-hormonal things to try, or do I need full HRT?
— Laura, Seattle, WA
Dear Laura,
First, thank you for writing in, and you’re definitely not alone. What you describe—the convergence of menopause transition, pelvic/urinary changes, and sexual-intimacy shifts—is becoming far more recognized as part of many women’s mid-life health stories.
Here’s Step-by-Step of Recommendations:
1. Clarify Your Status & Get Baseline Labs
Although you haven’t had a period for about a year (which often suggests you’re in menopause), it’s wise to confirm with your provider. Ask them to check your hormone levels. This helps map where your hormones are right now. Also, request a general health check—lipids, blood pressure, bone-density (if past 50), thyroid screen, iron / ferritin, vitamin D. Menopause doesn’t happen in isolation.
2. Separate & Track Your SymptomsHot Flashes + Night Sweats + Mood Shifts → Classic menopausal transition signs.
Ø Pelvic-Floor/Urinary Urgency → Menopause often leads to changes in the genitourinary tract: declining estrogen affects vaginal and urethral tissues, pelvic-floor muscle tone may drop, and urinary urgency or incontinence can appear.
Ø Sexual Changes → Decreased natural lubrication, changes in vaginal pH and elasticity, plus the pelvic/urinary issues can add discomfort or avoidance to intimacy.
3. Hormone Therapy (HRT) as a Key Tool—Not the Only Tool
Your concerns about HRT are valid—there’s been a lot of conflicting messaging over the years. But current thinking (and emerging regulatory change) is shifting toward more individualized assessment. In fact, this month, the FDA finally sided with updated science and removed the black box warning from HRT that previously cautioned about an increased risk of cardiovascular disease, breast cancer, and dementia.
For you:
Ø If you are otherwise healthy (no uncontrolled cardiovascular disease, active breast cancer risk, or major clotting issues), HRT can provide transformative relief for hot flashes, better vaginal/urethral trophic support, and indirectly help sexual health.
Ø The route matters: local vaginal estrogen (creams, rings, tablets) combined with systemic (patch/pill) if needed. The specific formulation and dose should be based on your symptoms, hormone levels, and risks.
Ø Ask your doctor: “What are my individualized risks/benefits given my age, health history, family history?”; “What formulation do you recommend and why?”; “How long would we plan to continue?”; “What monitoring will we do (e.g., mammogram, cardiovascular screening, bone density)?”
If HRT is contraindicated for you (due to history of hormone-sensitive cancer, clotting disorders, etc), then non-hormonal strategies become especially important.
4. Targeted Non-Hormonal & Complementary Supports
Even if you go ahead with HRT, or if you opt not to, you’ll benefit from supportive measures. Consider:
Ø Pelvic-Floor Physical Therapy: Strengthening, bladder-training, urgency-management techniques.
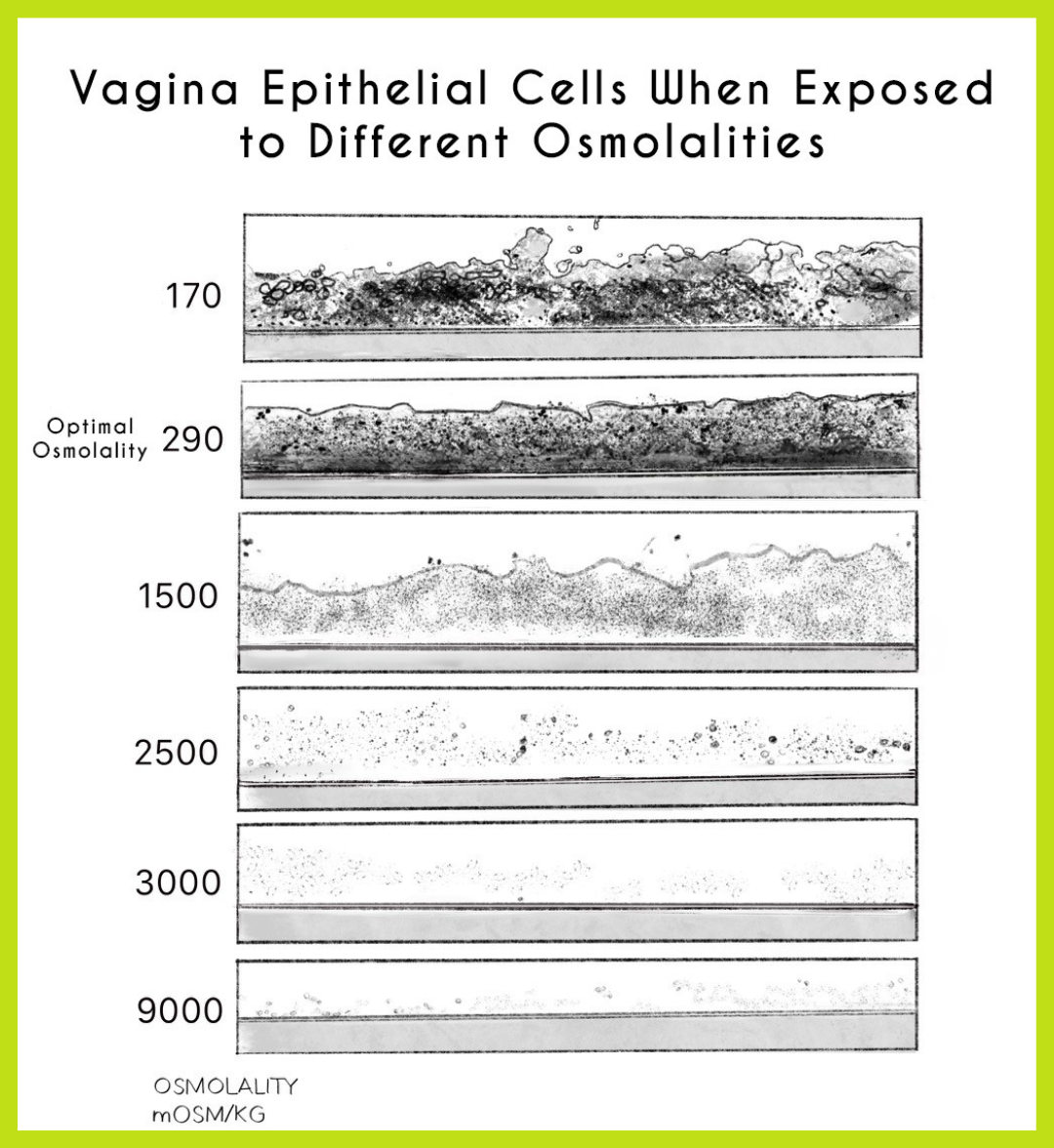
Ø Vaginal Health: Lubrication, such as an iso-osmolar, pH balanced vaginal moisturizers for sexual comfort (Desert Harvest Aloe Glide).
Ø Lifestyle: Regular resistance training (especially important post-menopause for muscles + bones), good sleep, stress management, nutrition
Ø Supplementation: Human bio-identical lactoferrin to support iron regulation, inflammation, bladder/vaginal mucosal health, and microbiome balance (Desert Harvest Bio-identical Lactoferrin); iron (as needed based on labs) for energy, thyroid function, and preventing deficiency or overload; vitamin D for bone, mood, immune, and muscle support; and calcium to maintain bone density and reduce osteoporosis risk during the menopausal transition.
Ø For Urinary Urgency: Bladder-retraining and reducing bladder irritants such as caffeine, artificial sweeteners, acidic foods.
Bottomline:
You’re at a pivotal transition point in your health—menopausal, pelvic/urinary and sexual changes all intersecting. The good news: you don’t have to accept these as “just what happens.” With a thoughtful plan that combines hormone support (if appropriate), pelvic/urinary care, and sexual wellness strategies, you can reclaim comfort, intimacy and vitality. Be your own advocate, ask the questions above, and lean on a provider who sees the whole picture (not just hot flashes or just bladder urgency).
Wishing you courage in this chapter—and here’s to feeling better, inside and out.
— Heather Florio, Health Columnist